Genicular Artery Embolization & Genicular Nerve Ablation For Osteoarthritis of Knee
Genicular Artery Embolization (GAE)
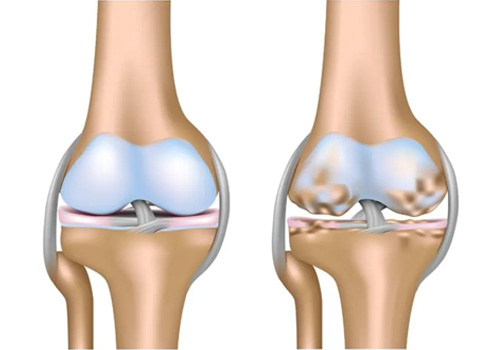
Genicular artery embolization (GAE), or embolization of the knee, is a novel minimally-invasive procedure providing immediate and long term pain relief for patients with osteoarthritis (OA), by reducing the blood flow to the lining of the knee, known as the synovium. It is performed by an Interventional Radiologist (IR), who is a specialist physician that uses X-rays and other imaging modalities to see in the body and treat diseases without surgery.
Treatment for: Osteoarthritis of the knee
Why it’s done:
GAE blocks the blood flow to the lining of the knee, known as synovium, that are inflamed. By blocking these arteries, there is a reduction in the amount of inflammation associated with osteoarthritis, a process that can help or eliminate the associated knee pain. While further research is needed, initial trials shows the promise this technique holds for patients with debilitating knee pain who are not ready or willing to undergo knee replacement surgery. While it may not treat the underlying cartilage destruction, evidence so far shows that this may be an effective way to manage the symptoms. In an article published in the Society of Interventional Radiology in March 2021, average pain scores decreased from eight out of ten before GAE to three out of ten within the first week.
How is GAE performed:
GAE is performed with moderate ‘twilight’ sedation as an outpatient procedure, meaning the patient will go home after the procedure. The procedure generally takes one to two hours. Our IR physicians will insert a small catheter (a thin hollow tube) into the artery of the patient’s upper thigh and, with the use of X-rays, guide the catheter to the arteries supplying the lining of the knee. Tiny particles are then injected through the catheter into these arteries, reducing the blood supply. This in turn reduces the inflammation associated with osteoarthritis, which alleviates the pain.
What happens after the GAE procedure:
Patients go home the same and in most cases, relief begins to occur in two weeks, as the inflammation in the lining of the knee is reduced, relieving the knee pain associated with osteoarthritis.
Genicular Nerve Radiofrequency Ablation
Genicular nerve radiofrequency ablation (GNRFA), including conventional, cooled, and pulsed techniques, has been used in the management of symptomatic knee osteoarthritis (OA). This new and innovative treatment option has the capacity to decrease pain and improve function and quality of life in certain patients. GNRFA is reserved for patients with symptomatic knee OA who have had failure of conservative treatment and have had failure of or are poor candidates for surgery. GNRFA has been shown to consistently provide short-term (3 to 6-month), and sometimes longer, pain relief in patients. GNRFA has been demonstrated to be safe to administer repeatedly in patients who respond well to this minimally invasive procedure.
GNRFA is a 2-step procedure. First, patients are given a diagnostic block under fluoroscopy or ultrasound guidance. Specifically, 1 mL of lidocaine is injected using a 20-gauge, 3.5-in (8.9-cm) spinal needle around the superior lateral, superior medial, and inferior medial genicular nerve branches. The diagnostic block is extra-articular. If the patient reports a ≥50% reduction in baseline pain for a minimum of 24 hours following the injection, then the patient is a candidate for genicular ablation. The osseous landmarks for the diagnostic block are exactly the same as for the ablation procedure. Both procedures are well tolerated in the office setting under local skin anesthesia or can be done in the operating room under conscious sedation using a low-dose sedative such as midazolam for anxious patients. General anesthesia is not required for GNRFA. This procedure is most commonly performed by interventional pain specialists but may also be performed by any physician with appropriate training. In some jurisdictions, physician assistants and nurse practitioners may perform this procedure subject to their supervision requirements.
Conservative treatment for symptomatic knee OA includes weight loss management, physical and aquatic therapy, bracing, lateral wedge insoles, transcutaneous nerve stimulation, nonsteroidal anti-inflammatory drugs in combination with a proton pump inhibitor, autologous blood-based therapies, and cortisone and hyaluronic acid injections1,2. Surgical treatment for symptomatic knee OA includes knee arthroscopy, high tibial osteotomy, total knee replacement, and unicompartmental knee replacement in patients without lateral compartment disease2. It should be noted that there is some evidence suggesting that steroid injection, viscosupplements, and arthroscopy are not effective for the management of knee OA.
